Myomectomy
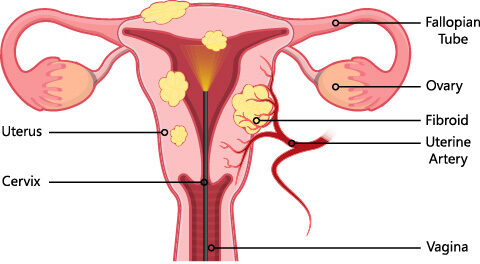
Myomectomy is the surgical removal of fibroids while leaving the uterus in place. Because a woman keeps her uterus, she may still be able to have children. If a woman does become pregnant after a myomectomy, the baby may need to be delivered by cesarean birth. Sometimes, though, a myomectomy causes internal scarring that can lead to infertility.
Myomectomy is a major surgical procedure, as major as a hysterectomy. The risks and recovery times are similar. A myomectomy is only done to preserve fertility in woman of reproductive age when future fertility is desired.
During myomectomy the position and size of the fibroids will be determined. At times removing all the fibroids could cause complications which make a hysterectomy unavoidable. If a hysterectomy is performed then a woman can not become pregnant. Some fibroids may be left in place in order to preserve the uterus to allow future pregnancy. The following video is an example of a robotic myomectomy performed by Dr. Genevieve Fairbrother.
Fibroids do not regrow after surgery, but new fibroids may develop. If they do, more surgery may be needed.
Myomectomy may be done in a number of ways:
Laparotomy
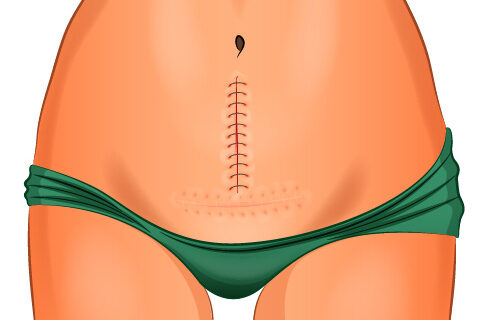
The method used depends on the location and size of the fibroids. In laparotomy, an incision (cut) is made in the abdomen. The fibroids are removed through the incision. In laparoscopy, a laparoscope is used to view the inside of the pelvis. Other tools are inserted through another small incision to remove the fibroids.
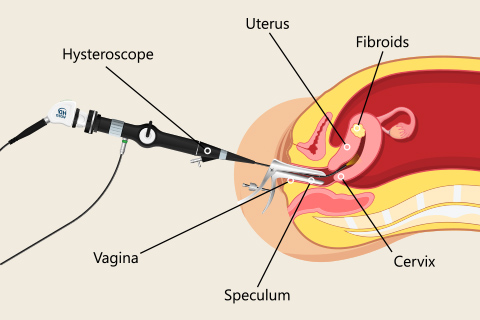
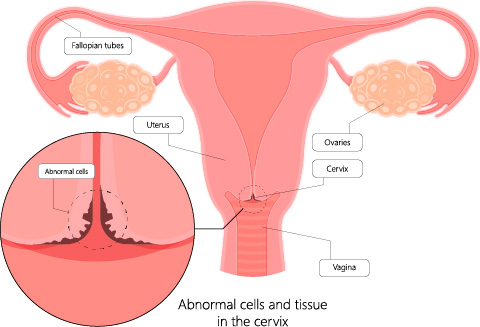
Hysteroscopy can be used to remove fibroids that protrude into the cavity of the uterus. A resectoscope is inserted through the hysteroscope. The resectoscope destroys fibroids with electricity or a laser beam. Although it cannot remove fibroids deep in the walls of the uterus, it often can control the bleeding these fibroids cause. In most cases, an overnight stay in the hospital is not necessary.
Myomectomy has risks, including bleeding and infection. Hysteroscopy may cause other problems related to the use of fluid during the procedure. Your doctor can explain all of the risks to you.
Preparing for Surgery
It is helpful to know what to expect before any major surgery. A physical exam is performed a few weeks before your surgery. Within 2 weeks of the surgery, a Preop Appointment is scheduled with your physician to discuss and finalize plans for the type of surgery to be performed and to be certain all questions are addressed.
Lab tests may be done at or after the preop appointment. A chest X-ray or electrocardiography (ECG) may need to be done for some patients.
Before any major surgery the use of all medications, including over the counter medicines, vitamins and supplements is reviewed to determine how they will affect the surgery. Some medications and supplements can cause complications during the surgery and may be discontinued on the day of surgery or earlier.
A laxative may be recommended before the day of surgery. Eat lightly the day before.
DO NOT EAT OR DRINK ANYTHING FOR 8 HOURS PRIOR TO SURGERY UNLESS SPECIFICALLY INSTRUCTED BY YOUR DOCTOR.
Some medications are given on the morning of surgery with a sip of water only.
On the day of surgery, the following things may happen:
- A needle is placed in the arm, wrist, or hand. It is attached to a tube called an intravenous (IV) line that will supply fluids, medication, or blood.
- An antibiotic to prevent infection.
- Special stockings or devices may be placed on the lower legs to prevent deep vein thrombosis (DVT). This condition is a risk with any surgery. Women at high risk of DVT may be given a drug to prevent blood clots from forming in the legs.
- Monitors will be attached before anesthesia is given. Either general anesthesia, which puts you to sleep, or regional anesthesia, which blocks out feeling in the lower part of your body will be used before the surgery begins.
- Pubic hair may be clipped. You may be awake or asleep while this is done.
- Before you are given anesthesia, you likely will be asked to state your name, the type of surgery you are having, or other information. This standard procedure, called a “time-out,” is done to ensure that the right surgery is being done on the right patient.
- A thin tube called a catheter will be placed in your bladder after you are comfortable. The catheter will drain urine from your bladder during the surgery.
What are the risks?
Myomectomy is a very common surgery, but is a major surgery. As with any surgery, problems can occur:
- Infection
- Bleeding during or after surgery
- Injury to the urinary tract or nearby organs
- Blood clots in the veins or lungs
- Problems related to anesthesia
- Death
Some problems related to the surgery may not show up until a few days, weeks, or even years after surgery. These problems include bowel blockage from scarring of the intestines or formation of a blood clot in the wound. These complications are more common after an abdominal hysterectomy.
Some people are at greater risk of complications than others. For example, someone with an underlying medical condition may be at greater risk for problems related to anesthesia. An assessment of risks for complications is made prior to surgery and preventive measures are taken. These risks are discussed with the doctor at the preop appointment.
Recovery
After a myomectomy, a person may need to stay in the hospital for a few days. The length the hospital stay will depend on the type of myomectomy performed.
A person is urged to walk around as soon as possible after your surgery. Walking will help prevent blood clots in the legs. They may receive medicine or other care to help prevent blood clots.
A person can expect to have some pain for the first few days after the surgery. They will be given medication to relieve pain. It is common to have some bleeding and discharge from the vagina for several weeks. Sanitary pads can be used after the surgery.
During the recovery period, it is important to follow recovery instructions carefully to allow proper healing. Be sure to get lots of rest, and do not lift heavy objects until your doctor says you can. Do not put anything in your vagina during the first 6 weeks. That includes douching, having sex, and using tampons.
Your doctor will help plan your return to normal activities. Slowly increase activities such as driving, sports, and light physical work. If you can do an activity without pain and fatigue, it should be okay. If an activity causes pain, discuss it with your doctor.
Our Locations
- NORTHSIDE OFFICE
 404-252-1137
404-252-1137
- EAST COBB OFFICE
 404-252-1137
404-252-1137
- JOHNS CREEK OFFICE
 404-252-1137
404-252-1137
- NORTHSIDE FORSYTH OFFICE
 404-252-1137
404-252-1137
Let's stay in touch
Our monthly newsletter keeps you up-to-date on healthy lifestyle, latest news, and our practice.