Urodynamics
Urodynamics refers to a group of procedures that are performed to examine voiding (urinating) disorders to determine the cause of a variety of bladder conditions. It is commonly obtained before treatment or surgery. The urodynamic test is a precise measurement using sophisticated instruments and is performed in our East Cobb office by our Nurse Practitioner, Dianne McMullen.

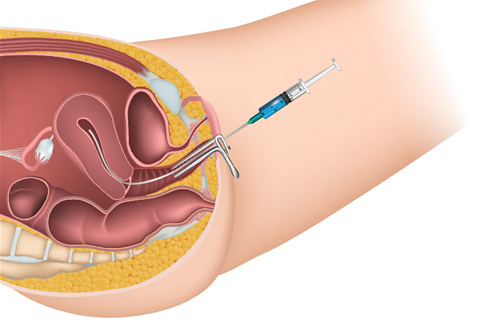
She will begin by asking you to urinate so she can measure how you empty your bladder. For the next part of the test, a small, flexible plastic catheter tube will be inserted into the opening of your bladder. Most patients say this is somewhat uncomfortable, but it shouldn’t hurt. A second small tube will be inserted into your vagina. These tubes are micro-measuring devices. Together they provide much useful information about the function of your bladder, your urethra (the tube the urine passes through when you urinate), and the muscles of your pelvis.
During the test, your bladder will be gradually filled with sterile fluid. As the bladder fills, a special monitor measures the pressure in your bladder. You may be asked to cough or bear down. If you have a bladder control problem, you may leak during this test. You should not be worried or embarrassed if that happens, since one of the main purposes of the test is to determine the cause(s) of leakage problems.
As your bladder is filled, you will inform us when you feel full enough that you would interrupt your activities to urinate, and then again when you feel completely full. After your bladder is completely full, another series of measurements will be made. The whole evaluation takes about 30-45 minutes.
Urodynamics is a simple, easy test that quickly looks at every aspect of bladder function. It will explain why a patient has the symptoms they do, and also can identify any other problems the current symptoms may mask. This information helps us form the treatment plan that is most likely to succeed in correcting your urinary problem.
Urodynamics helps us answer the following questions, which in turn will identify the type of leakage you have:
- Does the bladder react to filling appropriately?
- Does it store and empty, as it should?
- Is it overactive?
- Does the opening of the bladder open and close correctly?
- Is the bladder in the correct position, or has it dropped with pelvic floor weakening?
- If the bladder neck has dropped, has anything else dropped with it that needs to be addressed for treatment to be successful?
- Do the muscles of the pelvic floor contract, as they should?
This test very rarely causes any complications or problems. Less than 5% of women will develop a bladder infection after this test. Temporary irritation can occur after the examination, resulting in a feeling of burning with urination. (This usually only lasts a few hours and goes away without any treatment.) If you feel irritated after the procedure is over, we can recommend a medication. Other complications are extremely uncommon.
URODYNAMICS TESTING: THE COMPONENTS
Uroflowmetry
A uroflowmeter automatically measures the amount of urine and the flow rate (how fast the urine comes out). This creates a graph that shows changes in flow rate from second to second so the doctor or nurse can see the peak flow rate and how many seconds it took to get there. This test will be abnormal if the bladder muscle is weak or urine flow is obstructed.??The volume of urine is divided by the time to see what your average flow rate is. For example, 330 ml of urine in 30 seconds mean that your average flow rate is 11 ml per second.
Post void residual
After you’ve finished urinating, you may still have some urine, usually only an ounce or two, remaining in your bladder. To measure this urine, called a post-void residual, the nurse may insert a catheter into your bladder, drain the urine and measure it. A post-void residual of more than 200 ml (about half a pint) is a clear sign of a problem. Even 100 ml, about half a cup, may require further testing.
Cystometry (cystometrogram – CMG)
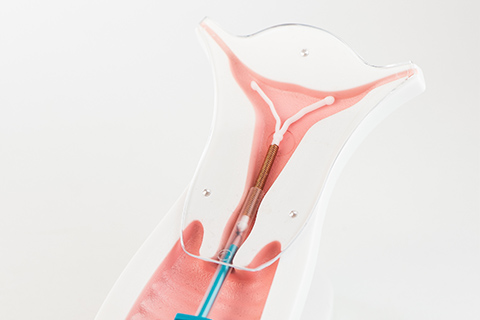
A cystometrogram (CMG) measures how much your bladder can hold, how much pressure builds up inside your bladder as it stores urine, and how full it is when you feel the urge to urinate. It tests both nerve and muscle function. The nurse will use a catheter to empty your bladder completely. Then a special smaller catheter with a pressure-measuring tube called a cystometer will be used to fill your bladder slowly with normal saline. Another catheter will be placed in the vagina to record pressure there as well. You will be asked how your bladder feels and when you feel the need to urinate. The volume of water and the bladder pressure will be recorded. You will be asked to cough or strain during this procedure. Involuntary bladder contractions can be identified.
While your bladder is being filled for the CMG; it suddenly may contract and squeeze some water out without warning. The cystometer will record the pressure at the time of the leak. This reading tells the doctor about the kind of bladder problem you have.
Valsalva leak point pressure
With your bladder comfortably full, you will be asked to exhale while holding your nose and mouth closed to apply abdominal pressure to the bladder, until you leak. These actions help the doctor or nurse evaluate your sphincter muscles.?
Urethral pressure profile
With thecatheter in place the doctor or nurse will slowly withdraw it from the bladder. This test determines the pressure in the urethra and it’s length. It is important to in distinguishing different types of stress incontinence. The result helps your doctor determine which surgical procedure is best for you. It is important that the bladder is stable so if your CMG test shows bladder spasms we may not do this part of the test until it has been corrected.
Pressure flow study
After the CMG, you will be asked to empty your bladder so that the catheter can measure the pressures required to urinate. This pressure flow study helps to identify bladder outlet obstruction. Bladder outlet obstruction is less common in women but can occur with a fallen bladder or rarely after a surgical procedure for urinary incontinence. Some catheters can be used for both CMG and pressure flow studies. We usually do not do this test unless you have an abnormal uroflowmetry or a high Post void residual.
Afterward
You might have mild discomfort for a few hours after these tests. Drinking two 8-ounce glasses of water each hour for 2 hours should help. Ask your doctor whether or not you can take a warm bath. If not, you may be able to hold a warm, damp washcloth over the urethral opening to relieve the discomfort.
Your doctor may give you an antibiotic to take for 1 to 2 days to prevent an infection. If you have signs of infection, fever, chills or pain, call your doctor.?
Results
For some of the more simple tests, you may get answers as the test is being done or right after it’s done. For others, it will take a few days. Your doctor will contact you with the answers.
PREPARING FOR URODYNAMICS TESTING
- Please do NOT apply lotions, powders, or sprays to the pelvic area on the day of your appointment.
- Please arrive 20 minutes prior to your scheduled appointment.
- Do NOT empty your bladder prior to the test. We would like your bladder “comfortably full” at the beginning of the test.?Do not empty just before the test, as it will delay getting started.
Please notify us in advance of your appointment if you think you might have a bladder infection, since your doctor will probably want to reschedule the test. Symptoms of a bladder infection might include burning or pain during urination, and foul smelling urine, or cloudy-colored urine. At the beginning of your test, we will check your urine for signs of infection and we may reschedule the test if infection is suspected.
Five days before the urodynamics stop any medications you might be taking to help your bladder function. Medicines you’d be asked to stop include detrol (tolterodine), ditropan (oxybutinin), probanthine (propantheline), tofranil (imipramine), urispas, dibenzyline, minipress, and cystospaz. We don’t want to measure the effect of these medications on your bladder. We want the test to measure your bladder’s problem without them. Stopping these 5-days before will ensure they are out of your system and don’t falsely affect the test results.
If one of your bladder medicines is elmiron, don’t stop that for the testing. (Elmiron doesn’t affect the test.) Do not stop your regular medications, such as heart, blood pressure or diabetic medications.
Let's stay in touch
Our monthly newsletter keeps you up-to-date on healthy lifestyle, latest news, and our practice.